Physiological blood clotting
A complicated cascade
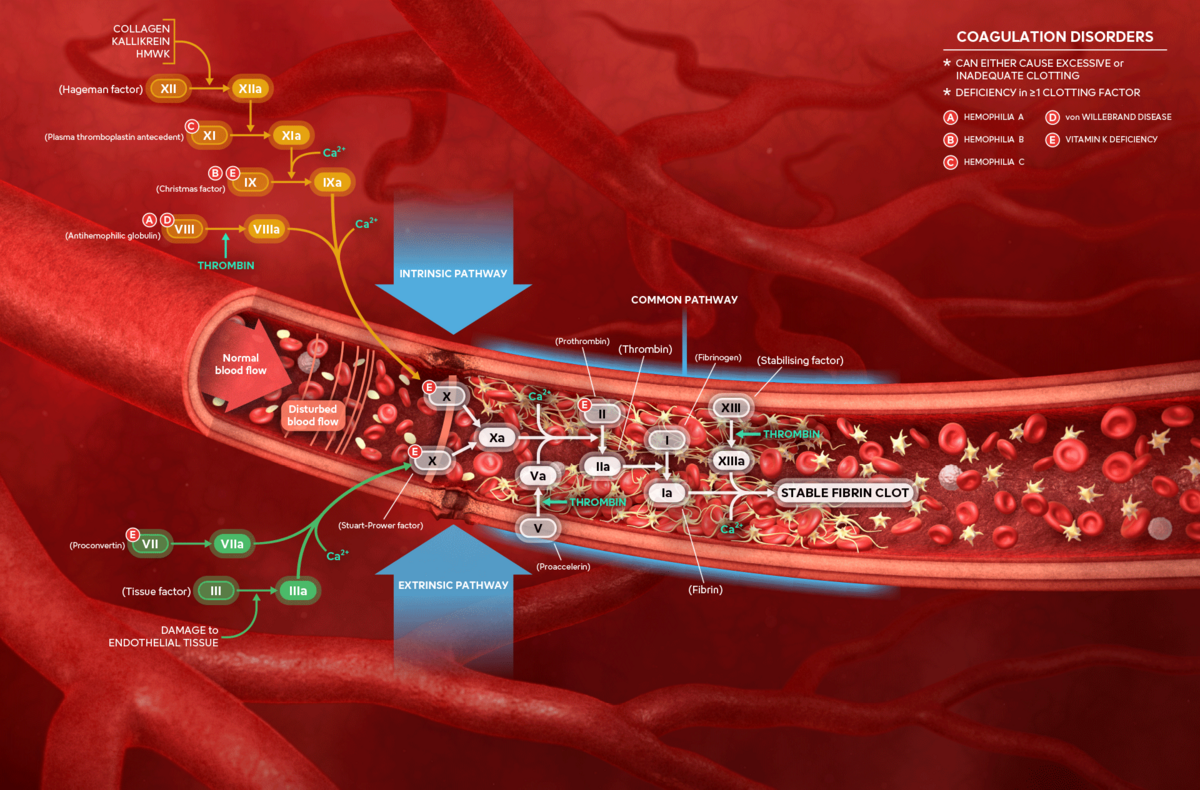
Blood clotting is a vital, multi-step process. When the blood vessel wall (endothelium) is damaged from the outside (extrinsic) due to injury or from within (intrinsic) due to disease, platelets (thrombocytes) initially seal the damaged site (‘white’ clot).
- The intrinsic pathway
Foreign or charged surfaces coming into contact with blood in the body trigger the intrinsic pathway of coagulation, which consists of specific clotting factors. - The extrinsic pathway
An injury (trauma) to tissue or the blood vessel wall (endothelium) exposes tissue factor, which triggers the extrinsic pathway of coagulation by activating specific clotting factors.
In the course of the blood clotting process, special proteins ensure that the initial platelet plug is transformed into a stable clot consisting of a cross-linked fibrin mesh and densely packed cells. This stable ‘red’ clot seals the injured tissue, allowing and promoting tissue repair and wound healing. These proteins, known as ‘clotting factors’, are interconnected through a complex reaction chain called the ‘coagulation cascade’.
Many clotting factors do not have individual names; they are simply labelled with Roman numerals. A lower case ‘a’ following the number indicates that the factor has been activated.
The final steps of the reaction chain have distinct names: prothrombin is the inactive precursor of thrombin, which ultimately converts fibrinogen into fibrin—the backbone of a stable clot.
Impaired blood clotting
Haemophilia – ‘bleeding disorder’
In healthy individuals, bleeding from small wounds lasts about 2 to 5 minutes. In haemophilia, blood clotting is significantly slower, and wounds take considerably longer to stop bleeding. Internal bleeding can also occur, potentially damaging organs, muscles, and joints as the bleeding simply won’t stop.
The best-known forms of haemophilia are Haemophilia A and Haemophilia B, both caused by a genetic mutation resulting in the absence of a specific clotting factor. Other forms of haemophilia are extremely rare.
- Haemophilia A
- Prevalence: 1 in 5,000 male individuals [1]
- Missing factor: VIII
- Haemophilia B
- Prevalence: 1 in 25,000 to 30,000 male individuals [1]
- Missing factor: IX
Haemophilia treatment – past and future
Until now, regular intravenous injections of the missing clotting factor in a concentrated form derived from healthy donors have been used to prevent prolonged bleeding in haemophilia patients. New factor concentrates with a prolonged half-life in the patient or so-called ‘clotting factor mimetics’ recently reduced the frequency of injections significantly. Now, a new treatment option – gene therapy – has the potential to significantly reduce the risk of severe bleeding and prevent or slow the progression of joint damage in the long term.
Haemophilia prevalence
Worldwide, the number of affected individuals – the vast majority being men – is estimated to be just over one million (with over 400,000 severe cases), though many remain undiagnosed. For the EMEA region (Europe, Middle East and Africa) with an estimated population of 2.2 billion people, this would amount to approx. 220,000 cases of haemophilia A, and roughly 37,000 cases of haemophilia B. [1, 2]
Men – the weaker sex?
Many genes responsible for clotting factors are located on the X chromosome. Females have two X chromosomes per cell, while males have only one. Therefore, a woman can usually compensate for a defective clotting factor gene with the intact version on her other X chromosome. A male, however, cannot.
References
[1] Berntorp E et al. (2021): Disease Primers Nature Reviews: 7: 45
[2] Duda H et al. (2020): The German Hemophilia Registry: Growing with its Tasks J. Clin. Med. 9, 3408